Professor Stefano Pagliara
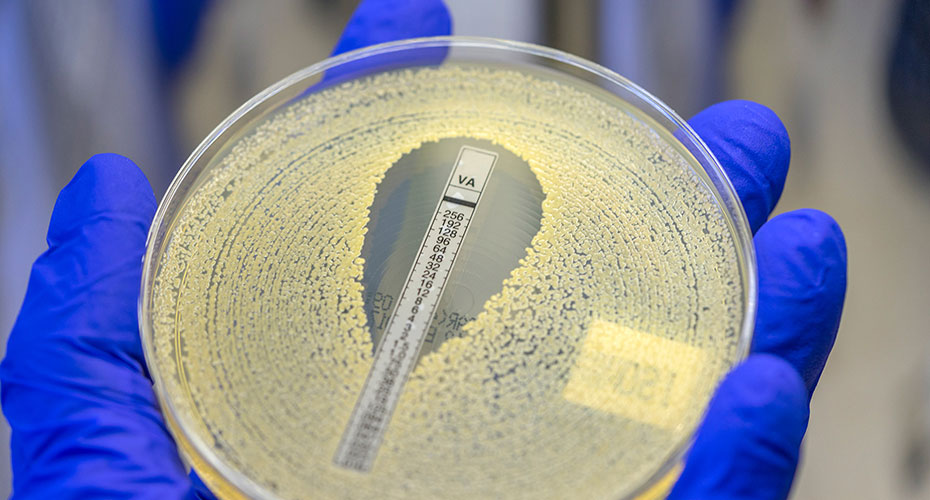
Stefano Pagliara is Professor of Membrane Transport in AMR at the University of Exeter. His research is focused on understanding how microbial cells interact with their environment both as a community and as individual cells with an emphasis on the transport of antibiotic molecules across bacterial membranes.
Besides standard microbiology techniques and omics approaches, his group develops bespoke microfluidic devices that enable us to accurately control the microenvironment surrounding the cells and measure antibiotic accumulation and efficacy on the very same cell. These cutting-edge capabilities allow his work to shed light on the molecular mechanisms underpinning AMR and to discover new therapies based on combinations of antibiotic molecules and bacteriophages.