Our precision approach to tackling Diabetes
Diabetes affects more than 460 million people globally. At the University of Exeter, we are making discoveries that are swiftly translated into healthcare, to improve lives worldwide.
Our unique precision diabetes approach focuses on getting the right treatment for each patient, as swiftly as possible. Our team has discovered 21 different genetic types of diabetes, excelled in improving diagnosis throughout the world, and optimised treatment for all diabetes types.
We are revolutionising healthcare around the world.
Discover how our vital research is helping clinical services treat diabetes.
In focus
Precision diabetes: The right treatment for each patient
The University of Exeter has led the way in making discoveries that are swiftly translated into healthcare, to improve lives worldwide.
"Our Precision Diabetes approach to research focuses on understanding the genetics and variations of diabetes and developing and communicating the best treatment options. This is absolutely crucial to getting the right diagnosis for patients and their families first time and avoiding harmful complications."
Professor Andrew Hattersley FRS
Professor of Molecular Medicine,
Consultant Physician

From gene discovery to revolutionising clinical care
When the Exeter diabetes lab was set up in 1995, medicine did not recognise that many forms of diabetes are caused by a single gene mutation.
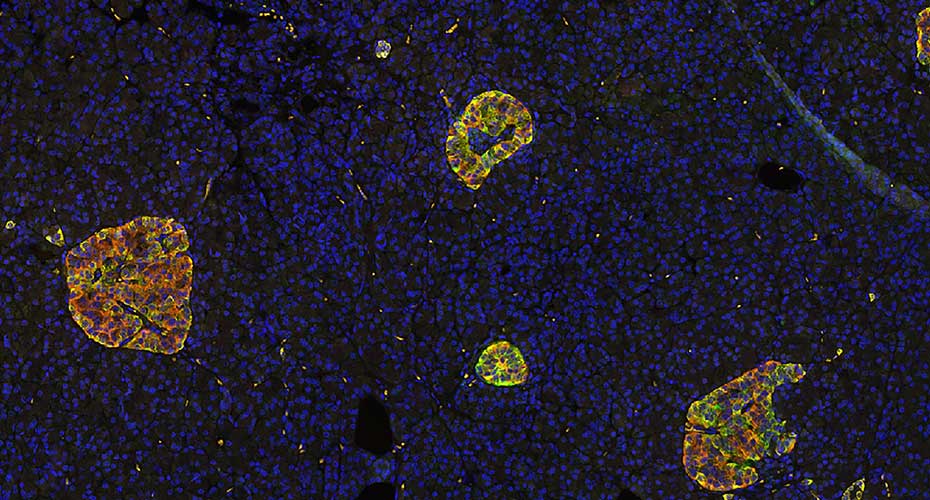
Unravelling the mysteries of the pancreas to improve type 1 diabetes diagnosis
Exeter have busted diagnosis myths and created new, simple and inexpensive diagnostic tests that are being used around the world.

Understanding type 2 diabetes, to treat all its forms
By far the most common form of diabetes, type 2 diabetes is nevertheless misunderstood. While classified as one condition, the complex disease actually comes in all shapes and sizes.
Research talent spotlight

Professor Andrew Hattersley FRS
Professor of Molecular Medicine,
Consultant Physician
Overview:
I am a clinical scientist, distinguished for my contributions to the understanding of the genetics of diabetes and the application of that knowledge to clinical practice. I became Gillings Chair in Precision Medicine in 2015, and lead the Precision Medicine initiative in Exeter working with both scientific and clinical colleagues. Professor Sian Ellard and I set up and head the premier international research team working on monogenic diabetes and I have played a major role in the UK research effort into the genetics of type 2 diabetes. My research combines state-of-the-art molecular genetics with physiological and clinical investigations in patients. I use the accidents of nature that cause monogenic diabetes to understand the critical role of the gene product in humans, in a similar fashion to many laboratory scientists who study knockout animals. A key theme of my approach is that scientific discoveries are rapidly and effectively translated into improvements in clinical care.

PhD training
High-quality PhD training is an urgent priority to ensure the next generation of researchers is equipped with the skills to make a real impact worldwide. Explore PHD study today.

Current vacancies
Following a recent major award, we are able to offer a number of diabetes research opportunities.
To enquire please email: diabetescareers@exeter.ac.uk.